In “Understanding the Impact of Diabetes on Pregnancy: Mother and Child Concerns,” we explore the intricacies of diabetes and its potential impact on pregnancy. Focusing on women who struggle with diabetes, we shed light on the concerns surrounding pregnancy and the potential effects it can have on both the mother and the child. By delving into this topic, we hope to provide a comprehensive understanding of the implications of diabetes on pregnancy, ultimately empowering women to make informed decisions and take necessary precautions.
In This Article
ToggleUnderstanding Diabetes and Pregnancy
Pregnancy can be an exciting and joyful time in a woman’s life, but for women with diabetes, there are additional considerations and potential complications to be aware of. Understanding the impact of diabetes on both the mother and the child is crucial for ensuring a healthy pregnancy and positive outcomes for both. In this article, we will explore the definition of diabetes, the prevalence of diabetes during pregnancy, and the different types of diabetes that can occur in pregnancy.
Definition of Diabetes
Diabetes is a chronic condition that affects the body’s ability to regulate blood glucose levels. There are several types of diabetes, but the most commonly known types are type 1 and type 2 diabetes. In type 1 diabetes, the body does not produce enough insulin, while in type 2 diabetes, the body’s cells become resistant to insulin. During pregnancy, there are specific types of diabetes that can occur, including gestational diabetes, which develops during pregnancy and usually resolves after childbirth.
Prevalence of Diabetes During Pregnancy
The prevalence of diabetes during pregnancy has been on the rise in recent years. According to the Centers for Disease Control and Prevention (CDC), approximately 2-10% of pregnant women in the United States are affected by gestational diabetes. It is important to note that women who already have diabetes before becoming pregnant are at an increased risk for complications during pregnancy.
Types of Diabetes in Pregnancy
During pregnancy, there are three main types of diabetes that can occur. Gestational diabetes, as mentioned earlier, develops during pregnancy and usually resolves after childbirth. However, women who have had gestational diabetes have an increased risk of developing type 2 diabetes later in life. Pre-existing diabetes refers to women who have diabetes prior to becoming pregnant. This includes women with type 1 or type 2 diabetes. The third type is a relatively rare form called “diabetes of pregnancy” or “overt diabetes.” This refers to women who have diabetes that is first diagnosed during pregnancy.
Impact of Diabetes on the Mother
When a woman with diabetes becomes pregnant, there are increased risks of complications that need to be considered. Managing diabetes during pregnancy is crucial for the health and well-being of both the mother and the developing fetus. Let’s explore some of the potential impacts of diabetes on the mother.
Increased Risk of Complications
Women with diabetes are at an increased risk for various complications during pregnancy. These may include high blood pressure, preeclampsia, preterm labor, and delivery, among others. Proper management of diabetes before and during pregnancy can help reduce the risk of these complications and ensure a healthier pregnancy.
Gestational Diabetes and Long-term Health
Developing gestational diabetes during pregnancy can have long-term health implications for the mother. Women who have had gestational diabetes are at a higher risk of developing type 2 diabetes later in life. Therefore, it is important for women with a history of gestational diabetes to adhere to a healthy lifestyle, including regular exercise and a balanced diet, to reduce the risk of developing type 2 diabetes in the future.

This image is property of images.pexels.com.
Impact of Diabetes on the Child
In addition to the potential risks for the mother, diabetes during pregnancy can also have significant impacts on the developing child. Let’s explore some of the potential effects that diabetes can have on the child.
Risk of Congenital Anomalies
Babies born to mothers with diabetes have a higher risk of developing congenital anomalies, such as heart defects, neural tube defects, and kidney problems. It is important for women with diabetes to closely manage their blood glucose levels before and during pregnancy to help minimize the risk of these complications.
Macrosomia (Birth of a Large Baby)
One of the concerns with diabetes during pregnancy is the increased likelihood of giving birth to a large baby, known as macrosomia. This occurs due to higher levels of glucose crossing the placenta, leading to increased fetal growth. Delivering a large baby can increase the risk of complications during birth, including shoulder dystocia (where the baby’s shoulders get stuck during delivery).
Neonatal Hypoglycemia
When a mother has diabetes, the baby’s pancreas may produce excess insulin in response to the elevated glucose levels in the mother’s blood. After birth, this can lead to low blood sugar levels in the baby, known as neonatal hypoglycemia. Regular monitoring of the baby’s blood glucose levels and appropriate management of feeding and glucose supplementation may be necessary to ensure the baby’s well-being.
Respiratory Distress Syndrome
Babies born to mothers with diabetes are at an increased risk of developing respiratory distress syndrome (RDS). RDS is a condition where the baby’s lungs are not fully developed and have difficulty functioning properly. Close monitoring and possible interventions, such as surfactant therapy, may be needed to help the baby breathe more effectively.
Long-term Effects on the Child’s Health
Children born to mothers with diabetes may be at higher risk of developing health issues later in life, such as obesity, type 2 diabetes, and cardiovascular disease. While genetics and lifestyle factors play a role, proper management of diabetes during pregnancy can help minimize these risks.
Preconception Counseling and Planning
Preconception care is crucial for women with diabetes who are planning to become pregnant. It involves managing blood glucose levels before pregnancy, making necessary medication adjustments, adopting healthy dietary and lifestyle changes, engaging in regular exercise and weight management, and screening for and managing any complications that may arise. Let’s explore these aspects in more detail.
Importance of Preconception Care
Preconception care aims to optimize a woman’s health and diabetes management before she becomes pregnant. This ensures that blood glucose levels are well controlled and that any potential complications are identified and managed early. It is recommended that women with diabetes who are planning to become pregnant seek preconception counseling to receive personalized guidance and support.
Managing Blood Glucose Levels Before Pregnancy
Achieving and maintaining target blood glucose levels before pregnancy is vital for the health of both the mother and the developing fetus. High blood glucose levels during early pregnancy can increase the risk of birth defects. Working closely with healthcare professionals to monitor blood glucose levels and adjust diabetes management strategies is essential in preparation for pregnancy.
Potential Medication Adjustments
Certain medications that are commonly used to manage diabetes may not be safe to use during pregnancy. It is important for women with diabetes to discuss their medications with their healthcare team to determine if any adjustments need to be made before pregnancy. Some women may need to switch from oral anti-diabetic medications to insulin therapy during pregnancy.
Dietary and Lifestyle Changes
Maintaining a healthy diet and lifestyle is crucial for managing diabetes during pregnancy. Women should aim to consume a balanced diet that includes a variety of nutrient-rich foods and limit their intake of refined sugars and processed foods. Regular exercise, such as walking or swimming, can also help manage blood glucose levels and promote overall well-being.
Regular Exercise and Weight Management
Engaging in regular exercise before and during pregnancy can help improve insulin sensitivity, manage weight gain, and reduce the risk of complications. However, it is important for women to discuss their exercise plans with their healthcare team to ensure their safety and to receive guidance on appropriate exercises during pregnancy.
Screening and Management of Complications
Women with diabetes should undergo regular screening for potential complications, such as eye and kidney problems, before becoming pregnant. If any complications are detected, appropriate management strategies can be implemented to reduce the risk of further damage and promote a healthier pregnancy.

This image is property of images.pexels.com.
Monitoring Blood Glucose Levels During Pregnancy
Monitoring blood glucose levels is a fundamental aspect of diabetes management during pregnancy. By closely monitoring blood glucose levels, pregnant women with diabetes can ensure that their levels are within the target range. Let’s explore the importance of monitoring, target blood glucose levels, and different methods of monitoring.
Importance of Monitoring
Monitoring blood glucose levels is crucial for managing diabetes during pregnancy. Regular monitoring allows pregnant women to identify patterns and make any necessary adjustments to their insulin therapy, medications, dietary choices, and overall diabetes management plan. This helps to maintain stable blood glucose levels and prevent complications.
Target Blood Glucose Levels
The target blood glucose levels during pregnancy may vary depending on individual factors and recommendations from healthcare professionals. Generally, the American Diabetes Association (ADA) recommends target ranges of 95 mg/dL (fasting) and 140 mg/dL (1 hour after meals). It is important for women to work closely with their healthcare team to establish their specific target ranges.
Methods of Monitoring
There are two main methods of monitoring blood glucose levels during pregnancy: self-monitoring of blood glucose (SMBG) and continuous glucose monitoring (CGM). Let’s explore these methods in more detail.
Self-Monitoring of Blood Glucose (SMBG)
SMBG involves using a glucose meter to measure blood glucose levels at various times throughout the day. Pregnant women with diabetes may be advised to perform SMBG before meals, after meals, and at bedtime. Regular monitoring can help identify patterns and guide adjustments to insulin therapy, dietary choices, and overall diabetes management.
Continuous Glucose Monitoring (CGM)
CGM is a more advanced method of blood glucose monitoring that provides continuous real-time readings throughout the day and night. A CGM system consists of a small sensor inserted under the skin, which measures glucose levels in the interstitial fluid, and a receiver or smartphone app that displays the readings. CGM can provide valuable insights into glucose trends and help pregnant women with diabetes make timely adjustments to their diabetes management plan.
Collaboration with Healthcare Professionals
It is important for pregnant women with diabetes to work closely with their healthcare team, including doctors, nurses, and diabetes educators, to establish a monitoring schedule and receive guidance on interpreting blood glucose readings. Regular communication and collaboration between the pregnant woman and her healthcare team can help ensure optimal blood glucose control and a healthier pregnancy.
Management Strategies for Diabetes During Pregnancy
Managing diabetes during pregnancy requires a comprehensive approach that includes tight glucose control, appropriate medication therapy, nutritional therapy, regular prenatal check-ups, and education and support. Let’s explore some of the key management strategies for diabetes during pregnancy.
Importance of Tight Glucose Control
Maintaining tight glucose control is crucial for reducing the risk of complications and ensuring a healthy pregnancy. Pregnant women with diabetes should work with their healthcare team to establish an individualized diabetes management plan that aims to keep blood glucose levels within the target range. This may involve adjustments to insulin therapy, oral anti-diabetic medications, and dietary choices.
Insulin Therapy
Insulin therapy is the most common treatment for pregnant women with diabetes. Insulin can help regulate blood glucose levels and provide the necessary fuel for the developing fetus. The healthcare team will work with the pregnant woman to determine the appropriate insulin regimen, dosage, and administration method. Regular monitoring of blood glucose levels is essential to determine the effectiveness of insulin therapy and make any necessary adjustments.
Oral Anti-Diabetic Medications
In some cases, pregnant women with type 2 diabetes may be able to continue taking oral anti-diabetic medications during pregnancy. However, certain medications are not safe to use during pregnancy and may need to be discontinued before conception or switched to insulin therapy. It is important for women to discuss their medications with their healthcare team to ensure the safety of both the mother and the developing fetus.
Nutritional Therapy
Nutritional therapy plays a significant role in managing diabetes during pregnancy. Pregnant women with diabetes should aim to follow a healthy and balanced diet that provides adequate nutrients for both the mother and the developing fetus. This may involve monitoring carbohydrate intake, portion control, and consuming a variety of nutrient-rich foods. Working with a registered dietitian or a diabetes educator can provide valuable guidance and support in developing a personalized meal plan.
Glycemic Index and Carbohydrate Counting
Understanding the glycemic index (GI) of foods and practicing carbohydrate counting can help pregnant women with diabetes make informed choices about their food intake. Foods with a low GI tend to have a smaller impact on blood glucose levels compared to foods with a high GI. By counting carbohydrates and knowing the GI of foods, pregnant women can better manage their blood glucose levels and maintain stable readings.
Regular Prenatal Check-ups
Regular prenatal check-ups are essential for monitoring the progress of the pregnancy and assessing the well-being of both the mother and the developing fetus. Pregnant women with diabetes should attend scheduled appointments with their healthcare team to ensure that their blood glucose levels, blood pressure, and other important health markers are within the target ranges. These check-ups also provide an opportunity to address any concerns or questions.
Education and Support for the Mother
Education and support are invaluable components of managing diabetes during pregnancy. Pregnant women with diabetes should receive comprehensive education on various aspects of diabetes management, including blood glucose monitoring, dietary choices, insulin therapy, potential complications, and self-care practices. Support from healthcare professionals, family, and peers can also help alleviate anxiety and provide a sense of community during this journey.
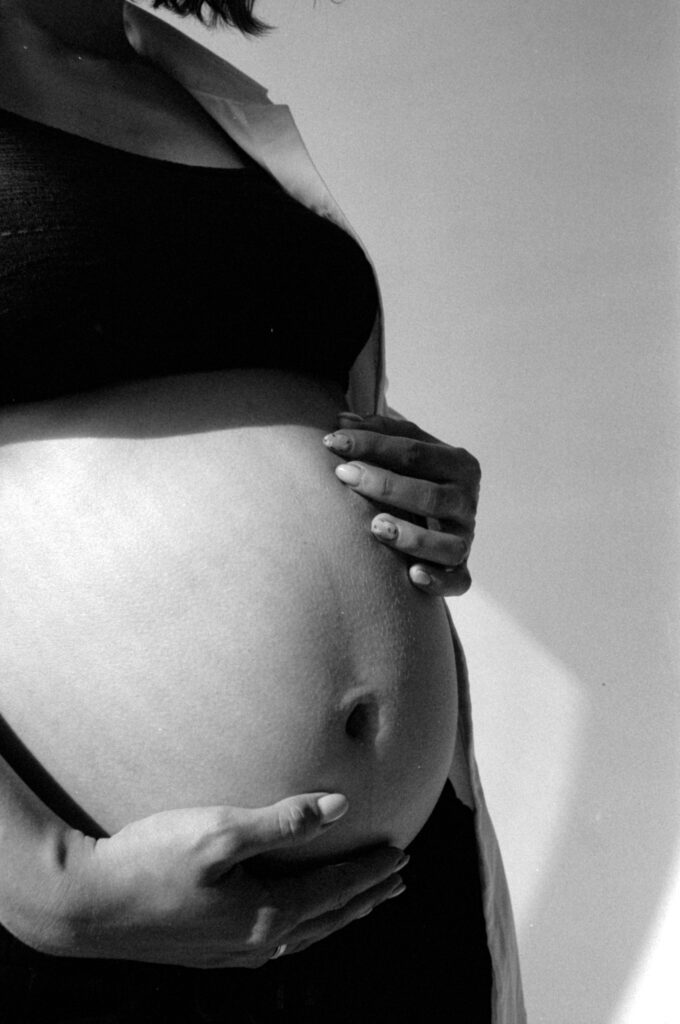
This image is property of images.pexels.com.
Potential Complications and Interventions
Despite vigilant diabetes management during pregnancy, there are still potential complications that may arise. Let’s explore some of these complications and the interventions that may be necessary.
Gestational Hypertension and Preeclampsia
Women with diabetes are at an increased risk of developing gestational hypertension or preeclampsia during pregnancy. These conditions can cause high blood pressure and damage to organs. Close monitoring of blood pressure, early detection of symptoms, and appropriate management strategies, such as medication, may be necessary to prevent complications.
Polyhydramnios (Excessive Amniotic Fluid)
Polyhydramnios is a condition characterized by an excess amount of amniotic fluid surrounding the baby during pregnancy. Women with diabetes have a higher risk of developing polyhydramnios. It is important to monitor fluid levels regularly and manage the condition carefully to reduce the risk of preterm labor and other complications.
Preterm Labor and Birth
Preterm labor and birth refer to the delivery of a baby before 37 weeks of gestation. Women with diabetes are at an increased risk of preterm labor and birth due to various factors, such as high blood pressure, polyhydramnios, and poor glucose control. Careful monitoring and interventions, such as medications to delay labor, may be necessary to prolong the pregnancy and give the baby the best chance of optimal development.
Induction of Labor
In some cases, healthcare professionals may recommend inducing labor for women with diabetes in order to manage potential complications. Induction of labor involves the use of medications or other techniques to initiate labor and delivery. The decision to induce labor is made based on various factors, such as blood glucose control and overall health of the mother and the developing fetus.
Cesarean Delivery
Women with diabetes may have an increased likelihood of needing a cesarean delivery (C-section) due to various factors, such as macrosomia, breech position of the baby, or other complications. A C-section involves surgically delivering the baby through an incision in the mother’s abdomen and uterus. Close communication between the healthcare team and the mother is essential to determine the most appropriate mode of delivery.
Neonatal Intensive Care Unit (NICU) Admission
Babies born to mothers with diabetes may require admission to the neonatal intensive care unit (NICU) for specialized care and monitoring. This may be due to complications related to diabetes, such as respiratory distress syndrome, low blood glucose levels, jaundice, or other medical conditions. The NICU provides around-the-clock care and support for newborns who need extra assistance during their first days or weeks of life.
Postpartum Care and Follow-Up
The postpartum period is a critical time for women with diabetes as they transition from pregnancy to motherhood. Proper postpartum care and follow-up are essential for monitoring blood glucose levels, promoting breastfeeding, managing diabetes, and ensuring the long-term health of both the mother and the child.
Monitoring Blood Glucose Levels After Delivery
After giving birth, it is important for women with diabetes to continue monitoring their blood glucose levels to ensure that they return to pre-pregnancy ranges. Regular monitoring in the postpartum period helps identify any fluctuations or trends that may require adjustments to diabetes management strategies. Close collaboration with healthcare professionals is crucial during this phase.
Breastfeeding and Diabetes
Breastfeeding is highly recommended for women with diabetes, as it provides numerous health benefits for both the mother and the baby. Breastfeeding can help regulate blood glucose levels in the mother, promote bonding, and enhance the baby’s immune system. Women with diabetes should work with lactation consultants and healthcare professionals to establish a successful breastfeeding routine while managing their diabetes.
Contraception Options
While it may seem premature to consider contraception options immediately after childbirth, it is crucial for women with diabetes to discuss family planning and contraception choices with their healthcare team. Certain contraceptive methods, such as hormonal methods, may have implications for blood glucose control and overall health. Open communication and personalized guidance can ensure that both the mother’s and the developing fetus’s health is protected.
Diabetes Management in the Postpartum Period
Managing diabetes in the postpartum period is essential for preventing long-term complications and maintaining overall health. Women with diabetes should continue to monitor their blood glucose levels, maintain a healthy lifestyle, and follow the recommended diabetes management plan established by their healthcare team. Regular follow-up appointments with healthcare professionals can provide valuable guidance and support during this phase.
Long-term Follow-up for Both Mother and Child
Long-term follow-up for both the mother and the child is critical to monitor their health and well-being. Women with a history of gestational diabetes or pre-existing diabetes should undergo regular screenings for diabetes and other related health conditions. Additionally, children born to mothers with diabetes may need ongoing monitoring for potential health issues as they grow. Collaborative care between healthcare professionals and the family is important to ensure optimal long-term outcomes.
Emotional and Psychological Support
Living with diabetes and navigating the challenges of pregnancy can have a significant impact on mental health and well-being. Emotional and psychological support play a vital role in helping women cope with the emotional challenges that may arise during this time. Let’s explore the importance of emotional support and the resources available to pregnant women with diabetes.
Impact of Diabetes on Mental Health
Living with diabetes, particularly during pregnancy, can be emotionally challenging. Women may experience increased stress, anxiety, and concerns about managing their diabetes effectively. It is important to acknowledge and address the impact of diabetes on mental health and seek appropriate support.
Coping with the Challenges of Diabetes and Pregnancy
Coping with the challenges of diabetes and pregnancy requires a multi-faceted approach. This may involve learning stress management techniques, seeking emotional support from loved ones, participating in support groups, and engaging in activities that promote relaxation and self-care. Each woman’s coping strategies will be unique, and it is important to find what works best for them.
Support Groups and Counseling Services
Support groups and counseling services can provide a safe space for pregnant women with diabetes to share experiences, seek guidance, and receive emotional support. These resources may be available through healthcare providers, community organizations, or online platforms. Participating in support groups can help women connect with others who are going through similar experiences and gain valuable insights and encouragement.
Partner and Family Support
The support of partners and family members is invaluable during diabetes and pregnancy. Partners and family members can play a significant role in providing emotional support, helping with diabetes management tasks, and understanding the challenges that arise. Open communication, empathy, and involvement in the healthcare journey can foster a supportive and nurturing environment for the pregnant woman.
Conclusion
Understanding the impact of diabetes on both the mother and the child during pregnancy is crucial for ensuring a healthy and successful outcome. By acknowledging the risks and taking proactive measures, women with diabetes can greatly improve their chances of a positive pregnancy experience and promote long-term health for both themselves and their children. A multidisciplinary approach, involving healthcare professionals, education, support networks, and personalized care, is key to achieving the best possible outcomes for women with diabetes during pregnancy and beyond.
Related posts:
 Long-Term Health Concerns for Women with Diabetes
Long-Term Health Concerns for Women with Diabetes
 Organic Apple Cider Vinegar Gummies with The Mother: Delicious Apple Flavor for Appetite Control, Metabolism Boost, Detox, and Energy Support – 60ct Vegan Gummies, USDA Certified & Non-GMO, No Artificial Ingredients
Organic Apple Cider Vinegar Gummies with The Mother: Delicious Apple Flavor for Appetite Control, Metabolism Boost, Detox, and Energy Support – 60ct Vegan Gummies, USDA Certified & Non-GMO, No Artificial Ingredients
 Vegan Nordic Apple Cider Gummies with The Mother Strain – 60 Count, No Vinegar Taste – Chewable ACV Supplement (Pack of 1)
Vegan Nordic Apple Cider Gummies with The Mother Strain – 60 Count, No Vinegar Taste – Chewable ACV Supplement (Pack of 1)
 Balancing Diabetes Management and Enjoyment through a Healthy Diet
Balancing Diabetes Management and Enjoyment through a Healthy Diet
 Coping with the Emotional Challenges of Living with Diabetes
Coping with the Emotional Challenges of Living with Diabetes
 Viynran 10 Inch Ceramic Portion Control Plates for Weight Management and Diabetes Control – Set of 2, Reusable and Microwave Safe
Viynran 10 Inch Ceramic Portion Control Plates for Weight Management and Diabetes Control – Set of 2, Reusable and Microwave Safe











No comment yet, add your voice below!